For a newborn to come out of the world from the darkness of the uterus, it is quite a daunting event. Although it has been breathing inside her mother’s womb, it has done so because of its mother. Once this baby is delivered, it has to learn how to breathe by itself.

Can you imagine how difficult it must be? And monitoring the changes that these newborns make from womb to the outside world is made easier through some standard pediatric procedures, one of which is almost always used by midwives, nurses, and doctors – the Apgar score.
The Apgar Score Defined

The long name for this test is the Newborn Scoring and Delivery – Apgar. Developed in 1952 by Dr. Virginia Apgar, it is a tool that assesses the performance of newborns when they are being delivered and how well they can cope and adjust after they are delivered.
It is important to note, however, that the Apgar score does not measure the newborn’s overall state. It merely provides some signs regarding the newborns’ breathing performance and blood circulation capabilities. Once a score falls below good on this test, then the medical staff can give some interventions as early as possible to improve their breathing.
Virginia Apgar had left a truly significant legacy when she created the Apgar score, although she was not only known for it. Her off-the-charts accomplishments include:
- She was a well-admired anesthesiologist.
- She was a leader in promoting the wellness of mothers and newborns.
- She was one of the only very few women who was accepted into the College of Physicians and Surgeons at Columbia University.
- She became the first woman who was accepted to work as a full-time professor at Columbia University.
- She was also the first woman to become chief of the Presbyterian Hospital.
On top of all of these, she made sure to allot time in pursuing her beloved hobbies such as stamp collection, fly fishing, and learning to fly planes.
Having mentioned all of that, it is also important to note that Dr. Apgar’s most significant achievement was the Apgar score.
How The Apgar Came To Be
As Dr. Virginia Apgar was observing the corners of the delivery room every time a baby was born, she noticed that the newborns were not receiving much care. Most of the nurses and midwives would immediately turn their focus to the mothers who just gave birth, and not much evaluation was given to the newborns. Dr. Apgar was not happy that they were struggling to breathe yet no one was there to find out how they were doing, and to think that during that time, most of the neonatal deaths were due to hypoxia, or not enough oxygen in the brain.
She concluded that neonatal deaths would be further decreased if attention was given on the newborns’ breathing, and an assessment was made during and after delivery, and she was right to the point. Fast forward today, after 65 years, the Apgar score is still widely used around the world.
The Acronym APGAR
Aside from its having originated from Dr. Apgar, the test was later improved and was given an acronym using the name itself. Here is what the letters stand for and their corresponding characteristics.

A is for Appearance of skin color. The baby’s skin tone should generally be pink or rosy, indicating normal oxygenation of blood. For darker-colored babies, the medical staff checks the palms of the hands, soles of the feet, and roof of the mouth. As mentioned also in MedLinePlus, if the skin color is pale or blue, it is a sign that the baby’s lungs and heart are not in its optimal function.
P is for Pulse or heart rate. The average neonatal pulse is more than 100 beats per minute. A nurse or other member of the medical staff measures this. A value of less than 100 should cause concern.
G stands for Grimace. Here, the baby’s reflexes are evaluated. A set of reflexes is performed by stroking the soles of the feet (Babinski), light pinch, and suctioning the sinuses. A positive reaction is a grimace, cough or sneeze, or a cry. A lack of these reactions may require mediation.
A is for Activity, which is an evaluation of the newborn’s muscle tone. The medical practitioner gently flexes and extends the baby’s upper and lower limbs, and usually, there’s resistance when doing this, meaning that the sound is strong. If, however, they are easily straightened without challenge, there is a need for medical intervention.
R is for Respiration, where the medical team measures the baby’s breathing performance. When there is an irregularity, such as the baby gasping for air, then immediate help is required.
Understanding Apgar Scoring Results
Here’s how and when the Apgar is taken:
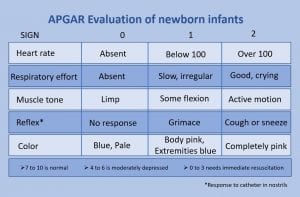
When the baby comes out, the nurse, doctor, or another member of the medical team assess the baby using the categories listed above. For all five parts, the team evaluates and then scores the baby using a scale of 0 to 2 – 2 being the highest and most ideal presentation for that category of the test.
When the team is done evaluating and scoring the five categories, they add all the scores to come up with a total, which ranges between 0 and 10. Usually, scores are below 10, as the newborn has just come out and undergone trauma. This is the reason why the test is repeated five minutes after the baby’s birth. Below is a scoring chart, which will enlighten you on how the points are appointed.
| 0 Points | 1 Point | 2 Points | |
| Appearance | Blue or pale or body | Pale or blue hands and feet, but the rest of the body has a pink tone | Pink body, hands, and feet. |
| Pulse | No pulse | Less than 100 beats per minute | 100 beats or more per minute |
| Grimace | No response | Twisted or crumpled facial expressions when the face is stimulated | Crying, coughing, or sneezing in addition to grimacing |
| Activity | Slack, limp extremities | Some flexing of the extremities | Strong flexing of the extremities in addition to some resistance in attempts to straighten their arms or legs |
| Respiration | Not breathing | Slow, irregular | Strong cry, regular breaths |
Interpreting the Apgar Scores
The three classifications used when interpreting Apgar scores are reassuring, moderately abnormal, and low. A score of 7 and above is classified as comforting or usual. However, it is essential to remember that despite having a high score the first time the baby is evaluated, the test always needs to be repeated on the fifth minute mark.
When the score is low at the first test and then shows a reassuring or normal score at the fifth minute, this means that the interventions administered by the medical team have been effective, and the baby has successfully adjusted. If, however, the scores are consecutively low on the first and fifth minute of taking the test, more effort on giving efficient intervention must be required. Also, the Apgar test may be needed every five minutes for a total of 20 minutes under these circumstances.
A moderately abnormal result gives a score of 4 to 6, and a score of 0 to 3 is classified as low.
Conclusion – The Relevance Of The Apgar Score

When the score on the fifth minute of evaluation remains low, there is also a possibility of several severe complications for newborns. However, it should be noted that the Apgar score alone couldn’t detect complications such as cerebral palsy. Ultimately, it is an essential tool in determining whether or not the baby can adjust well to the outside world when he comes out, and the prime factor used is breathing.
The Apgar score can also be used to decide whether or not additional medical care is needed when the baby comes out into the world.
FAQs On Apgar Scoring Results
How do you interpret Apgar scoring results?
Apgar scoring results can be interpreted by looking at the number ranges. Scores 7-10 indicate that you have a healthy baby; scores 4-6 say that you need to get their health checked.
What does an Apgar score of 4 mean?
If the Apgar scoring results to 4, it merely states that your infant is in a poor health condition. You need to consult a doctor at once to know what’s wrong with them.
What does an Apgar score of 3 indicate?
An Apgar score of 3 is extremely worrying as it indicates that your child’s life is in danger. A lot of infants who get such a result require immediate resuscitation.
Why is the Apgar scoring system important?
Apgar scoring system is essential because it serves as a health screening tool for newborns. Without it, professionals may not be able to tell whether the baby that they have helped to deliver is healthy or not.
What is considered a low Apgar score?
A low Apgar score goes from 0 to 6. However, a single low score should not worry you immediately since things can normalize after a few minutes.
When is the Apgar score checked?
Medical professionals check the baby’s Apgar score one minute and five minutes after they enter the world. Nurses usually announce it both times in the labor room.
How do you remember Apgar?
Medical students and professionals use mnemonics to remember Apgar. Also, the closer the score is to 10, the better the infant’s condition is.
What does Apgar mean in medical terms?
Apgar stands for Appearance, Pulse, Grimace, Activity, & Respiration. Nurses provide a score for each on a scale of 0 to 2.
What is the Apgar assessment?
The Apgar score is used by doctors to assess a newborn’s pulse, appearance, movements, and breathing pattern. Any of these things can indicate how healthy a baby may be (read further here: https://www.whattoexpect.com/first-year/your-baby-s-apgar-tests.aspx).
Why are two Apgar ratings given?
The Apgar score is checked twice after one minute and five minutes of birth. The reason is that they want to see if the initial results will change after five minutes.
Last Updated on January 12, 2023 by Rejie Salazar
DISCLAIMER (IMPORTANT): This information (including all text, images, audio, or other formats on FamilyHype.com) is not intended to be a substitute for informed professional advice, diagnosis, endorsement or treatment. You should not take any action or avoid taking action without consulting a qualified professional. Always seek the advice of your physician or other qualified health provider with any questions about medical conditions. Do not disregard professional medical advice or delay seeking advice or treatment because of something you have read here a FamilyHype.com.